INTRODUCTION
Electronic prescribing (e-prescribing) is defined as the secure electronic creation of a prescription and its transmission between an authorized prescriber and the patient’s pharmacy of choice, using a clinical electronic medical record (EMR) and pharmacy management software (PMS).1 Various benefits can be realized through the use of e-prescribing, including a reduction in transcription errors, improved communication between prescribers and pharmacists, support for opioid safety strategies, and support for medication management.2 In Canada, several e-prescribing services are available reflecting a mix of national, provincial, and retail pharmacy enabled e-prescribing solutions. This bulletin shares findings and learning from an analysis of incidents involving e-prescribing in the community pharmacy setting, to inform continuous quality improvement.
BACKGROUND
It is recognized that some e-prescribing services include functionality to create an electronic prescription (e-prescription) within the EMR. Other e-prescribing services are limited to the transmission of the e-prescription as created in the prescribing module of the EMR. Depending on the e-prescribing service, e-prescriptions can 1) be transmitted directly from a prescriber’s EMR to the PMS of the patient’s chosen pharmacy, or 2) be retrieved by the pharmacy from a central or cloud-based repository.3
METHODOLOGY
Medication incidents associated with e-prescribing were extracted from 3 ISMP Canada databases (National Incident Data Repository for Community Pharmacies, Individual Practitioner Reporting, and Consumer Reporting*) for the 5-year period between August 1, 2018, to July 31, 2023. The search terms† “digital prescribing”, “telehealth”, “PrescribeIT”, “CPOE”, and “provincial”, along with variations of the term “e-prescribing” (appearing in the incident report description field) were used for the extraction. Incidents that did not result from e-prescribing (as defined above) and those that did not occur in the community setting were excluded.
QUANTITATIVE FINDINGS
Of the 312 incidents extracted and screened for inclusion, 87 incidents were included in the final analysis. The majority (91%) of these incidents were classified as near misses or as resulting in no harm. The remaining 9% were reported as mild harm (i.e., temporary harm to the patient).
The medication-use stages most frequently involved were order entry (76%) and prescribing (30%). Some incidents were reported to involve more than one medication-use stage. The top 5 types of errors identified in submitted reports are shown in Figure 1.
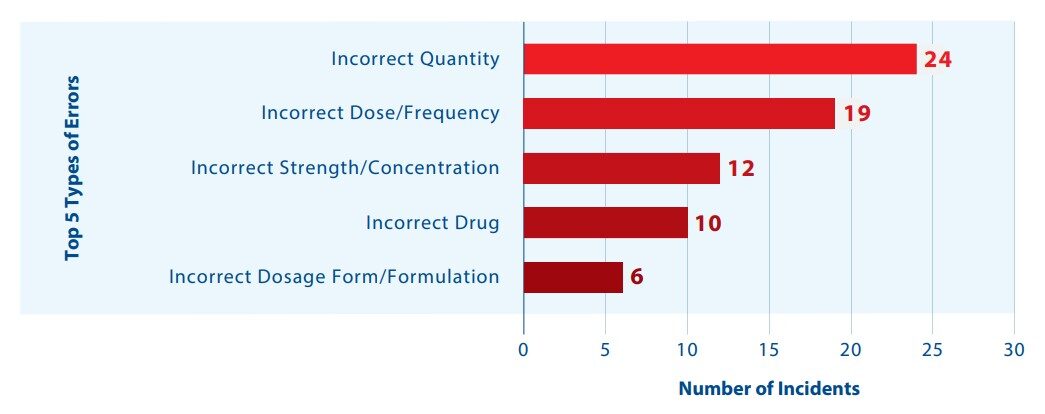
FIGURE 1. Top 5 types of errors reported in the multi-incident analysis.
QUALITATIVE ANALYSIS
Two distinct themes were identified in the qualitative analysis, along with several subthemes, as shown in Figure 2.

FIGURE 2. Themes and subthemes identified in the qualitative analysis.
THEME: Prescription Creation Errors
Incorrect Entry/Data Selection in Key Data Fields
Several incidents described incorrect entries in the “product”, “directions on the prescription label (SIG)”, or “quantity” fields when e-prescriptions were created. These reports included prescribers selecting the incorrect product from the list available in the prescribing module of the EMR software. A key contributing factor was an inability to find the intended product in the drug list. Errors in multi-step directions for use were also reported and resulted from difficulty finding the corresponding entries for selection (e.g., when titrating or tapering doses). Other errors described prescribing an incorrect number of tablets.
Incident Example: An e-prescription was received for dexamethasone 4 mg tablets with instructions to take 8 mg by mouth daily for 2 weeks. The quantity on the e-prescription incorrectly stated 14 tablets, when the required quantity was 28 tablets.
Conflicting Entries in Free-Text Field
The field for free-text notes in e-prescriptions allows prescribers to convey additional prescription-related information not captured in other fields. Using this free-text field for information that belongs elsewhere in the record (e.g., the directions-for-use field) or for details that are contradictory to other information in the prescription can create confusion, may disrupt workflow, and can potentially lead to patient harm.4 In several of the reported incidents, information in the free-text field contradicted instructions elsewhere on the prescription, or the free-text information was overlooked by pharmacy staff because it would typically be captured in a specific data field.
Incident Example: A prescriber sent an electronic prescription for bupropion 300 mg, with a message in the notes field to stop a previous prescription for bupropion 150 mg. The pharmacy team members did not see this note.
TIP: Prescribers
Use the “cancel prescription” feature, if available, rather than the notes field to discontinue prescriptions.
TIP: Pharmacy Teams
Review all components of a prescription, including the notes field.
TIP: PMS Providers
Consider incorporating a visual cue to indicate that data have been entered in the notes field.
THEME: Architecture and Interoperability Challenges
Lack of Prescription Notification Alerts
Several of the reported incidents described pharmacy staff not being aware of new e-prescriptions or dose changes, which led to delays in treatment. Reports also identified a need for pharmacies to ensure that e-prescriptions are incorporated into regular workflows, with recognition that pharmacies continue to receive paper prescriptions, faxed prescriptions, and telephone orders.5
Incident Example: Pharmacy team members were unaware of updated e-prescriptions. The patient received their medications in a blister pack, and the most recently filled pack did not reflect changes in the updated prescriptions. The errors were discovered when the next set of blister packs were due to be filled.
TIP: e-Prescribing Service Providers
Consider incorporating an alerting system when medications are updated or changed.
Incompatibilities with Pharmacy Software
One of the key advantages of e-prescribing lies in the integration of the prescriber’s prescription entry workflow in the EMR with the pharmacy’s dispensing workflow in the PMS. Ideally, information from the EMR is transmitted to the PMS without the need for transcription or modifications by the pharmacy team.6 This analysis found that seamless transmission of prescription information between the prescriber (EMR) and the pharmacy (PMS) does not always occur.
Reported difficulties with the interface and technology connection included instances when pharmacy staff had to manually enter information, or print prescriptions in order to read all the information in the data fields. Reporters also shared instances when prescribed quantities of controlled drugs did not match the days supplied or when the quantities changed during the entering and filling process. It was reported that some pharmacy teams are routinely printing these e-prescriptions before filling, to double check the prescribed and authorized quantities.

TIPS: EMR, PMS and e-Prescribing Service Providers
- Continue to work together to identify improvement opportunities for seamless transmission of prescription information between the EMR and PMS.
- To support verification, consider adding an image that displays the created prescription; team members can then view a detailed image alongside the data entry fields.
Incorrect Prescription Modifications during Pharmacy Order Entry
Transcription errors may occur when modifications to the prescription are required. This can occur, for example, when the prescribed item is not available at the pharmacy because of a drug shortage. Factors reported to contribute to prescription modification errors included distractions, confirmation bias, and look-alike medication names.
Incident Example: An e-prescription was submitted for “Prozac 20 mg”. The e-prescription information would typically auto-populate the PMS, but this did not happen because ‘Prozac’ was not active in the PMS list. As a result, the pharmacist had to manually enter the product name. “Paroxetine 20 mg” was inadvertently selected instead of “fluoxetine 20 mg”. The error was noticed during the final prescription check.
TIP: Pharmacy Teams
Whenever possible, incorporate independent double checks by a second pharmacy team member at key steps in the workflow.7 When working alone, establish a process whereby a delayed self-check of new prescriptions is routinely conducted at a later time.8
CONTINUED LEARNING FROM RECENT REPORTS
Several recent reports of incidents from consumers described opportunities for improved patient engagement in the prescription and dispensing processes. For example, reports described visits with the prescriber, during which e-prescriptions were sent directly to the pharmacy. Without a copy of the prescription, the patient or caregiver was not well-positioned to provide an extra check at pick-up and before use.
TIP: EMR and e-Prescribing Service Providers
Include user-friendly functionality that supports prescribers in providing patients with a copy of the e-prescription, or sharing prescription information via secure messaging.
TIP: Prescribers
Offer patients a copy of their e-prescription. Alternatively, share a copy of the prescription information in a secure message to the patient.2,9
Recent reports from stakeholders provide additional tips for improvements with e-prescribing.
TIPS: EMR, PMS and e-Prescribing Service Providers
- Develop improved electronic messaging between prescribers and pharmacy teams; for example, a confirmation of “message read”.
- Develop an alert that documents when prescriptions were dispensed, but not picked up by the patient.
- Bundle prescriptions for the same patient, rather than as multiple individual messages to support prescription workflow.
CONCLUSION
The use of e-prescribing continues to increase, offering safety benefits and convenience for prescribers, pharmacists, and patients. As with any new health care technology, there can be opportunities for error. Learning from reports of incidents related to e-prescribing supports continuous quality improvement and optimization of e-prescribing to enhance patient safety.2
![]()
The Canadian Medication Incident Reporting and Prevention System (CMIRPS) is a collaborative pan-Canadian program of Health Canada, the Canadian Institute for Health Information (CIHI), the Institute for Safe Medication Practices Canada (ISMP Canada) and Healthcare Excellence Canada (HEC). The goal of CMIRPS is to reduce and prevent harmful medication incidents in Canada.
Funding support provided by Health Canada. The views expressed herein do not necessarily represent the views of Health Canada.

The Healthcare Insurance Reciprocal of Canada (HIROC) provides support for the bulletin and is a member owned expert provider of professional and general liability coverage and risk management support.

The Institute for Safe Medication Practices Canada (ISMP Canada) is an independent national not-for-profit organization committed to the advancement of medication safety in all healthcare settings. ISMP Canada’s mandate includes analyzing medication incidents, making recommendations for the prevention of harmful medication incidents, and facilitating quality improvement initiatives.
Report Medication Incidents (Including near misses)
Online: ismpcanada.ca/report/
Phone: 1-866-544-7672
ISMP Canada strives to ensure confidentiality and security of information received, and respects the wishes of the reporter as to the level of detail to be included in publications.
Stay Informed
Subscribe to the ISMP Canada Safety Bulletins and Newsletters.
This bulletin shares information about safe medication practices, is noncommercial, and is therefore exempt from Canadian anti-spam legislation.
Contact Us
Email: cmirps@ismpcanada.ca
Phone: 1-866-544-7672
©2025 Institute for Safe Medication Practices Canada.
