INTRODUCTION
Many pediatric prescriptions are considered off label because the medications have not been reviewed and approved by Health Canada for pediatric use.1 When a medication prescribed for a pediatric patient is not commercially available in a suitable formulation, the pharmacy may need to compound the medication, or the caregiver may need to manipulate an adult product. This bulletin describes 2 recently reported incidents involving pediatric prescriptions and the need for system improvements.
INCIDENT #1
Clonidine was prescribed off label as 0.025 mg (25 mcg) for a pediatric patient. The patient had difficulty swallowing tablets or liquids, therefore the pharmacy consulted the prescriber and compounded the medication in a gummy formulation. During the preparation process, a 1000-fold error was made with clonidine powder, such that each gummy contained 25 mg instead of 25 mcg of clonidine. The child chewed the first gummy briefly before spitting it out, but then experienced hypotension and bradycardia leading to hospitalization.
INCIDENT #2
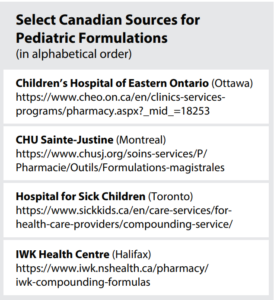
A medication was prescribed off label to treat a seizure disorder in a young child who could not use an alternative medication. The pharmacist did not have a compounding formula and, considering the balance of risks, provided instructions to the parents to cut the tablet into quarters to obtain the child’s required dose. In the incident report, the parent described the daily struggle of carefully splitting the small tablet (Figure 1) into quarters to get the prescribed dose, mixing the dose into food, and coaxing the child to eat all the food to ensure a full dose was ingested.

FIGURE 1. Size of the prescribed tablet (circled in red) relative to the millimeter markings on a ruler. (Adapted photo courtesy of the reporter)
BACKGROUND
The current Canadian federal regulations do not require pediatric data from manufacturers for medications likely to be used in children.2,3 In the United States (US) and the European Union (EU), manufacturers are required to obtain pediatric data in such situations.4,5 The low return on investment for manufacturers (due to Canada’s small population), the lack of pediatric-specific regulatory guidance for manufacturers, and delayed provincial/territorial reimbursement programs for pediatric formulations may contribute to the lack of commercially available products in Canada.2 A recent publication showed that 48% of the medications compounded in a Canadian pediatric hospital were commercially available as child-friendly formulations outside of Canada.6
When a medication is prescribed for an infant or child and there is no suitable commercially available pediatric formulation, either an adult dosage form or the active pharmaceutical ingredient (API) bulk powder must be manipulated to create the final product.7 Compounding involves multiple steps and calculations, with increased risks related to drug stability, therapeutic efficacy and product safety.8,9
Devastating consequences of compounding errors involving pediatric formulations,10,11 have informed safer compounding practices as described in the National Association of Pharmacy Regulatory Authorities’ (NAPRA) recent model standards.12 Many Canadian jurisdictions are implementing NAPRA’s standards. System safeguards to reduce risk of errors during compounding are also described in the Medication Safety Self-Assessment (MSSA) focused on “Never Events” in community pharmacy.
DISCUSSION
In the 1000-fold error described in the first incident, the dose was prescribed as 0.025 milligrams [mg].* During the compounding process, there was a mix-up when converting the unit of measure of clonidine powder from milligrams to grams for the formula sheet. The final weight of clonidine per gummy was 0.025 grams (instead of 0.025 milligrams). Previously, recommendations have been made and implemented to use clonidine tablets instead of powder when preparing pediatric oral liquids.11 Tablet-based formulas for clonidine suspension are readily available to help prevent errors.13,14 There is an opportunity to explore if this safeguard might also be applied to the formulation of gummies.
The anti-seizure medication in the second incident is commercially available as an oral liquid in both the US and the EU, but not in Canada.15 Availability of a commercial formulation such as a liquid facilitates accurate measurement of the small doses typically required for pediatrics.
In a 2018 pan-Canadian study, hospital pharmacists identified clonidine and several anti-seizure medications as the compounded pediatric oral formulations most in need of commercialization in Canada.16 Yet several years later, pharmacy compounding is still required for many of these medications.17 Commercially manufactured products are produced under stricter quality controls and therefore carry a lower risk of error than custom-made products.
RECOMMENDATIONS
The following strategies are recommended to meet the needs of pediatric patients.
Health Canada
- Update the regulatory framework to require pediatric product submissions (supported by Canadian pediatric studies or foreign data) when use of the medication in pediatrics is anticipated.3
- Develop clear pediatric-specific guidance to support manufacturers in meeting regulatory requirements.2
Provincial / Territorial Public Drug Programs
- Coordinate the product reimbursement decision with Health Canada’s approval process to minimize the time during which the commercial product is available (and therefore, in accordance with regulations, can no longer be compounded) and when it is reimbursed for patients.
Prescribers
- When prescribing medications that are not approved for pediatric use (i.e., off label), discuss with parents the risks and benefits. Offer comparable therapeutic alternatives, if possible.
- Include the patient’s weight on the prescription and the weight-based dosing parameters (e.g., micrograms per kilogram for clonidine) to facilitate additional checks by the pharmacist.
- Write out the medication strength in full, without abbreviations, where additional clarity would be helpful (e.g., milligram or microgram for clonidine doses). Communicate the dose as an amount or strength, not as a volume (in milliliters [mL]) and not as a fraction of a tablet.
- Transition to the use of electronic or computer generated prescriptions to reduce the risk of misinterpretation associated with handwritten and verbal prescriptions.
Pharmacy Managers, Pharmacists, and Pharmacy Technicians
- Communicate with the prescriber to ensure awareness of the need to compound the medication into a pediatric-friendly formulation. Offer comparable therapeutic alternatives, if possible, and compound only when the benefits outweigh the potential risks.
- Use standardized master formulas that are well-established, reviewed regularly, include the rationale for ingredient choices, and use units of measure that are consistent within and between electronic systems.11 For medications that can be dosed in micrograms, the use of commercially available tablets or capsules should be considered when developing the master formula. This will reduce the opportunity for 1000-fold errors that have occurred when weighing API powders.
- Update pharmacy dispensing software and master formulas to include an alert for compounded clonidine prescriptions. For example, “1000-fold dose errors have occurred with clonidine; triple check calculations and weights”.
- Require and document, on a standardized worksheet, a signed independent double check for every compounded product. The NAPRA Guidance Document for Pharmacy Compounding of Non-Sterile Preparations provides detailed guidance.12
- Use modern equipment (e.g., a digital scale) that is accurately calibrated and clearly displays the units of measure. A scale that prints the weight allows for a documented check.
- Implement use of unique identifiers for ingredients as part of the compounding process; examples include drug identification number (DIN) or Chemical Abstracts Service (CAS) number, and automated identification (e.g., bar code scanning).
- Input or update the patient’s weight into the pharmacy system before entering a new prescription for a pediatric patient. Have a scale (programmed to read in kilograms) available in the pharmacy to weigh pediatric patients, if needed.
- Activate or request alerts in the pharmacy software to highlight doses that exceed the maximum pediatric dose based on weight.
- Minimize the need for the child’s caregiver to manipulate the product to deliver the correct dose. For example, for a dose that is half of the tablet, offer to cut tablets at the pharmacy instead of dispensing whole tablets for the caregiver to cut at home.
Organizations Developing Master Formulas
- Publish formulas in easily accessible reference sources. Consistent, widespread use of validated, standardized formulas (with a specific set of standardized concentrations per medication) will support safe compounding practices and allow opportunities for continuous improvement.
- Develop formulas that incorporate commercially available dosage forms when appropriate (e.g., for medications that can be dosed in micrograms).18 The risk of error can be reduced by minimizing the need to weigh small amounts of an API.
CONCLUSION
In both incidents described above, the lack of a suitable pediatric formulation resulted in the need to provide an alternative form of the medication; there were harmful or potentially harmful patient outcomes. This bulletin provides recommendations and strategies for Health Canada, provincial/territorial public drug programs, prescribers, and pharmacy staff, as well as organizations involved in the development of compounding formulas. The aim is to advance the availability of commercial pediatric formulations, as well as the safety of compounded products.
![]()
The Canadian Medication Incident Reporting and Prevention System (CMIRPS) is a collaborative pan-Canadian program of Health Canada, the Canadian Institute for Health Information (CIHI), the Institute for Safe Medication Practices Canada (ISMP Canada) and Healthcare Excellence Canada (HEC). The goal of CMIRPS is to reduce and prevent harmful medication incidents in Canada.
Funding support provided by Health Canada. The views expressed herein do not necessarily represent the views of Health Canada.

The Healthcare Insurance Reciprocal of Canada (HIROC) provides support for the bulletin and is a member owned expert provider of professional and general liability coverage and risk management support.

The Institute for Safe Medication Practices Canada (ISMP Canada) is an independent national not-for-profit organization committed to the advancement of medication safety in all healthcare settings. ISMP Canada’s mandate includes analyzing medication incidents, making recommendations for the prevention of harmful medication incidents, and facilitating quality improvement initiatives.
Report Medication Incidents (Including near misses)
Online: ismpcanada.ca/report/
Phone: 1-866-544-7672
ISMP Canada strives to ensure confidentiality and security of information received, and respects the wishes of the reporter as to the level of detail to be included in publications.
Stay Informed
Subscribe to the ISMP Canada Safety Bulletins and Newsletters.
This bulletin shares information about safe medication practices, is noncommercial, and is therefore exempt from Canadian anti-spam legislation.
Contact Us
Email: cmirps@ismpcanada.ca
Phone: 1-866-544-7672
©2025 Institute for Safe Medication Practices Canada.
