“No Drug Selected” = Taking the Smart Out of Smart Pumps
Smart pumps with dose error reduction software (DERS) support organizations in creating a tailored library of medications with associated dosing guidelines. By establishing dosing limits and alerts within DERS, organizations can use smart pumps to detect dosing and programming errors that may harm patients. This safety bulletin outlines situations in which bypassing the drug library and DERS takes the “smart” out of smart pumps. It also describes the risks associated with bypassing this software and offers strategies to increase the use of this technology
INTRODUCTION
Smart pumps represent a significant advancement in the safety of parenteral medication administration.1 Smart pumps with dose error reduction software (DERS) support organizations in creating a tailored library of medications with associated dosing guidelines. By establishing dosing limits and alerts within DERS, organizations can use smart pumps to detect dosing and programming errors that may harm patients. This safety bulletin outlines situations in which bypassing the drug library and DERS takes the “smart” out of smart pumps. It also describes the risks associated with bypassing this software and offers strategies to increase the use of this technology.

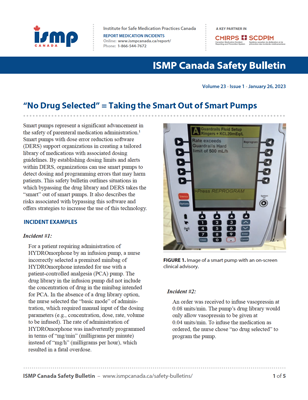
FIGURE 1: Image of a smart pump with an on-screen clinical advisory.
INCIDENT EXAMPLES
Incident #1:
For a patient requiring administration of HYDROmorphone by an infusion pump, a nurse incorrectly selected a premixed minibag of HYDROmorphone intended for use with a patient-controlled analgesia (PCA) pump. The drug library in the infusion pump did not include the concentration of drug in the minibag intended for PCA. In the absence of a drug library option, the nurse selected the “basic mode” of administration, which required manual input of the dosing parameters (e.g., concentration, dose, rate, volume to be infused). The rate of administration of HYDROmorphone was inadvertently programmed in terms of “mg/min” (milligrams per minute) instead of “mg/h” (milligrams per hour), which resulted in a fatal overdose.
Incident #2:
An order was received to infuse vasopressin at 0.08 units/min. The pump’s drug library would only allow vasopressin to be given at 0.04 units/min. To infuse the medication as ordered, the nurse chose “no drug selected” to program the pump.
BACKGROUND
The DERS is the foundation of smart pump safety features. Drug libraries incorporating DERS typically include the following features:2
- Available medications in commonly used or standardized concentrations • “Soft” dosing limits (which can be overridden) and “hard” dosing limits (which require reprogramming; example provided in Figure 1)3
- “Soft” dosing limits (which can be overridden)and “hard” dosing limits (which require reprogramming; example provided in Figure 1)3
- Bolus-dose, and possibly loading-dose, options
- Clinical advisories (e.g., requirement for an independent double check, reminder to change intravenous tubing after a certain period of time)
- Pump auditing capabilities (e.g., number and types of overrides, number of uses involving the “no drug selected” function)
Choosing “no drug selected”, “other drug”, “drug X”, “basic mode”, or a generic “IV fluids” (depending on the pump model) bypasses the smart pump’s drug library and DERS features. This type of workaround necessitates manual entry of the infusion rate and volume for the selected medication. Staff report using this function when the drug, concentration, or dose needed for a particular patient is not available in the drug library, when they are dealing with an emergency situation, or when the device-user interface is complex.4,5 Choosing to not use the safety technology associated with DERS—by overriding an alert or administering a dose that is outside the prespecified dosing limits—increases the risk of programming-related errors and potential patient harm.4 Importantly, when the drug library and DERS are bypassed, the smart pump is unable to identify any pump programming errors.4
DISCUSSION
In each of the incidents described above, the desired drug concentration or infusion rate was not available in the drug library. As a result, nurses chose the “basic mode” or “no drug selected” option in the smart pump, which necessitated manual programming of the infusion dosing parameters. The following factors can contribute to this type of workaround:
- Lack of standardization among prescriber orders (e.g., lack of predefined order sets).
- Lack of standardization among prescriber orders (e.g., lack of predefined order sets).
- Lack of alignment among organizational protocols, order sets, intravenous infusion manuals, drug libraries, and infusion practices.
- Complacency related to frequent use of the “no drug selected” function.
- Lack of appreciation for potential errors and patientharm when pump safety features are bypassed.
Smart pumps can capture extensive audit details about how these devices are being used, including use of the drug library, frequency of alert types, action taken in response to an alert (e.g., reprogramming for hard limits), and frequency with which soft limits are overridden.3 Analyzing pump audit data allows organizations to gain greater understanding of the use of the pumps and to optimize the safety benefits that such pumps offer.6,7
RECOMMENDATIONS
Nursing Leaders
- Develop a timely process to support end-users when incorrect or missing drug library settings are identified, as well as a clear process to remedy the concern.
- Implement a process to regularly (e.g., weekly or monthly) solicit and respond to feedback from nurses regarding the use of the “no drug selected” or equivalent function.
- Work with relevant multidisciplinary teams to ensure that drug libraries reflect current evidence, as well as local dosing practices for each specialty area.
- Provide initial and ongoing education to the nursing team and clients who will manage delivery of medications via pumps. For example, include tips for mental estimation to validate the medication dose programmed.
Pump End-Users
- Ask a colleague to provide an independent double check when administering high-alert medications.7
- Provide feedback to clinical leaders and/or pharmacy about incorrect or missing drug library settings. This can include use of reporting systems or other established mechanisms.
Organization Management
- Create a culture of safety that supports reporting and learning.
- Develop a quality improvement plan that utilizes available pump audit data to improve infusion pump safety.
- Regularly update organizational policies and protocols, intravenous infusion manuals, order sets, safeguards, and education associated with the safe use of infusion pumps to incorporate learning from incident reporting and analysis.
- Enable wireless and real-time updating of drug libraries so that pumps reflect the most recentversion of organizational protocols, order sets, and best practice.7
- Consider developing interoperability between smart pumps and electronic systems (e.g., electronic health records [EHRs], computerized physician order entry [CPOE], and electronic medication administration records [eMARs]) to allow the pump to be wirelessly pre-populated with infusion parameters from the EHRs and infusion data to be sent back wirelessly to the EHR.5
CONCLUSION
Incidents have been reported in which drug libraries with DERS have been bypassed during infusion pump programming, resulting in harm to patients. A key contributing factor is the misalignment between orders and drug libraries, which leads to workarounds. Practitioners in all disciplines should engage with those who build and regularly review and update drug libraries to ensure alignment of these devices with organizational protocols, order sets, and best practices. A timely process to support end-users when they identify challenges with pump programming or missing drug library settings and a clear process to remedy any concerns are key to optimizing safety with smart pumps.
![]()
The Canadian Medication Incident Reporting and Prevention System (CMIRPS) is a collaborative pan-Canadian program of Health Canada, the Canadian Institute for Health Information (CIHI), the Institute for Safe Medication Practices Canada (ISMP Canada) and Healthcare Excellence Canada (HEC). The goal of CMIRPS is to reduce and prevent harmful medication incidents in Canada.
Funding support provided by Health Canada. The views expressed herein do not necessarily represent the views of Health Canada.

The Healthcare Insurance Reciprocal of Canada (HIROC) provides support for the bulletin and is a member owned expert provider of professional and general liability coverage and risk management support.

The Institute for Safe Medication Practices Canada (ISMP Canada) is an independent national not-for-profit organization committed to the advancement of medication safety in all healthcare settings. ISMP Canada’s mandate includes analyzing medication incidents, making recommendations for the prevention of harmful medication incidents, and facilitating quality improvement initiatives.
Report Medication Incidents (Including near misses)
Online: ismpcanada.ca/report/
Phone: 1-866-544-7672
ISMP Canada strives to ensure confidentiality and security of information received, and respects the wishes of the reporter as to the level of detail to be included in publications.
Stay Informed
Subscribe to the ISMP Canada Safety Bulletins and Newsletters.
This bulletin shares information about safe medication practices, is noncommercial, and is therefore exempt from Canadian anti-spam legislation.
Contact Us
Email: cmirps@ismpcanada.ca
Phone: 1-866-544-7672
©2025 Institute for Safe Medication Practices Canada.